
In recent years, there have been several articles published that discuss the concept of “athlete’s heart,” which is comprised of either scarring or enlargement of the heart tissue over time. There is still a debate about whether or not this is harmful to the athlete; nevertheless, these stories have sparked a discussion among the endurance community about the importance of protecting one’s heart.
Tissue scarring is not the only possible side effect of exercise. In this article, we discuss another heart-based symptom and cause to consider: heart palpitations (arrhythmia) resulting from abnormal levels of electrolytes.
Palpitations, while not always harmful, can be unnerving and can feel like the heart is “skipping a beat,” beating too fast or fluttering. They have many causes, including high levels of caffeine, an allergic reaction, thyroid issues and even pregnancy. In the realm of endurance sports and for endurance athletes, however, one must consider electrolyte levels as well.
It is also important to distinguish between heart palpitations (the generalized feeling of a heartbeat that is rapid, fluttering, skipping, etc.. ) that can have many causes, and atrial fibrillation (AFib). This occurs when rapid electrical signals cause the heart’s two upper chambers to contract very fast and irregularly (referred to as an arrhythmia).
One of the symptoms of AFib are palpitations, but having palpitations does not necessary invoke AFib. The manifestation of AFib causes blood to accumulate in the upper heart rather than pumping into the heart’s two lower chambers as it normally would. The condition can be very serious and can lead to stroke and heart failure if left untreated. AFib can be temporary, persistent or permanent, and generally requires a physician’s diagnosis and treatment.
The purpose of electrolytes
Electrolytes are crucial to a variety of physiological functions. In particular, sodium, potassium, calcium and magnesium work together to help the body manage neurological impulses, muscular contraction, nutrient transportation, blood pressure and the sweating process. Electrolytes contain electric charges (thus their name), and these charges allow them to move in and out of cell walls, change the electric potential of cells, and conduct electrical impulses.
A change in the electrolyte content in blood is one of the potential triggers of heart palpitations.
To get an idea of how important electrolytes are to the exercise process, consider a 2016 study in Spain that examined 26 triathletes who raced a 70.3 distance triathlon. Half of the athletes were given sports drinks and the other half were given both sports drinks and electrolyte capsules, designed to replace 70 percent of sodium lost during the course of the race.
The triathletes who consumed extra electrolytes finished their race, on average, 26 minutes faster than the group who consumed sports drinks alone. To read more about this study, go here.
For the purpose of this blog post, the role of electrolytes in neurological signals and muscular contraction is mainly of interest, specifically in understanding how the heart requires electrolytes to function.
Electrolytes and the heart beat
“When treating congestive heart failure, one must consider how to prevent depletion of electrolytes or how to replete potassium and magnesium in deficiency states,” conclude the authors of a 1992 study published in Methods and Findings in Experimental and Clinical Pharmacology. Their conclusion is due to the fact that electrolytes are vital to the heart’s ability to contract.
Dr. Peter Kas of resus.com in Australia does an excellent job of explaining this process, which is summarized below.
Known as extracellular ions, sodium and calcium mainly exist in the body outside the cell walls. When sodium and calcium cross the cell wall, a cell becomes positively charged due to the positive charge of these electrolytes.
Potassium, as an intracellular ion, has the opposite effect as it moves towards the outside the cell. During a heart beat, these three electrolytes enter and exit the heart’s muscular cells in phases, resulting in changes to the electrical charges of these cells, which are measurable with an ECG, although easier to understand with the Overall Electrical Charge graph below.
First, sodium enters the cell, resulting in a net positive charge and spike. This positive charge is then maintained as calcium quickly follows, so the charge graph registers a mostly flat line. Finally, potassium exits through the cell wall and the original charge of the cell is restored. This last step is not as quick as step one, so the rate illustrated by the repolarization charge line is slower.
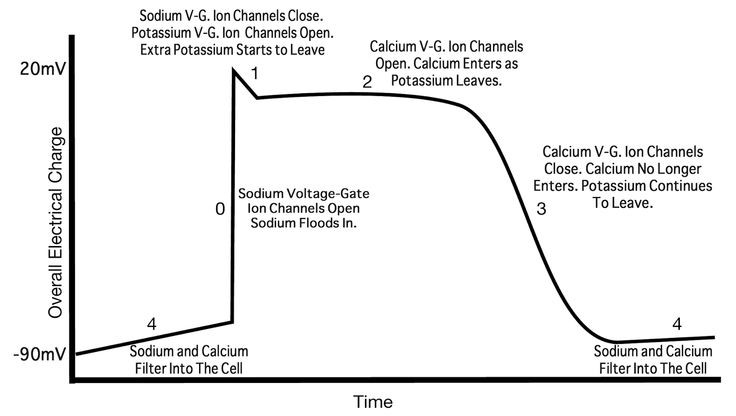
Image source: http://thepad.pm
Overall Electrical Charge graph converts to an ECG like this:
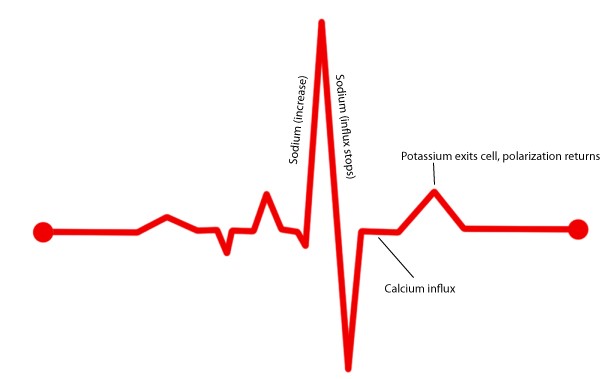
Image source: SaltStick
The corresponding ECG pattern will take place only when electrolytes are properly balanced. If one of the ions exists in too high or too low a concentration, the pattern will diverge.
Low potassium, known as hypokalemia, results in a slower repolarization of the cell, so the second spike will be too low. Hyperkalemia, or too much potassium, has the reverse effect. Sodium concentrations will have the same effect on the first spike in the ECG pattern.
Calcium’s effect is a little more complicated, but it nevertheless leaves distinct marks when there is too much or too little present in the heart.
These interruptions to a cell’s electrical pattern result in abnormal contractions of the heart muscle, and to an athlete, this can manifest itself is as heart palpitations. In these cases, the proper chemistry of the heart must be restored to counteract the negative symptoms.
Of course, non-athletes can experience abnormal levels of electrolytes as well, and the next section lists two case studies published in the Methodist DeBakey Cardiovascular Journal, which detail the physical symptoms and solutions to electrolyte imbalances.
Case study 1: Potassium
The first example describes the treatment of a 75-year old man who entered the emergency room complaining of heart palpitations, among other symptoms. After finding his potassium levels too low, the doctors prescribed an aldosterone blocker in attempt to prevent excessive potassium losses through urine. Aldosterone is a hormone that directs the kidneys to filter potassium out of the body, and too much aldosterone results in potassium levels that are too low.
Note that the exact method here is not that important, as potassium levels can be influenced by a number of hormones and physiological processes; it just so happens that in this case, the man’s aldosterone levels were too high.
The point is that potassium levels were abnormally low, which impacted the patient’s heart beat. Once potassium blood levels returned to normal, the patient’s blood pressure stabilized and his heart palpitations disappeared.
Case study 2: Magnesium + Calcium
In this case, a 36-year old woman, who earlier in her life had undergone intense chemotherapy to treat a bout of cancer, entered the hospital complaining of cramping and heart palpitations. The physicians measured the magnesium content of her urine and found it to be quite high, meaning her body was failing to absorb magnesium from her diet.
The doctors did not find an exact cause for the patient’s hypomagnesemia (low magnesium levels), but they assumed it was a side effect of the chemotherapy drug used to treat the patient’s cancer.
In addition to a host of physical problems such as cramping, low magnesium levels can affect both calcium and potassium levels in the body. After physicians returned the patient’s magnesium levels to normal through a combination of drugs and supplements, the patient’s symptoms went away.
Conclusion
These case studies and technical explanation demonstrate that electrolytes are not just useful to an endurance athlete; they are crucial. Sitting at the very center of aerobic activity — cardiovascular performance — electrolytes must remain in balance in order for the body to perform optimally.
While the body is adept at maintaining homeostasis under most conditions, significant demands (such as hot conditions, long distance training or racing) or dietary needs (due to training or racing) can disrupt these biological systems.
Provided an athlete’s diet contains sufficient amounts of these electrolytes, the body absorbs sodium, potassium, calcium and magnesium as needed. For day-to-day activity, athletes can maintain normal levels by eating a diet rich in fruits, vegetables, whole grains and legumes. During periods of long, intense exercise or periods of extreme heat, additional supplementation may be necessary.
The point of this article is not to say that all heart palpitations in an athlete are necessarily caused by out-of-balance electrolyte levels. As mentioned earlier, arrhythmia has many potential causes, including electrolyte imbalance.
There is often no way to know what is causing the arrhythmia, and the provided recommendations are on the list of things to do (which include proper sleep, reduce emotional stress, no alcohol, etc.) if you want to do everything you can to keep arrhythmia at bay. The point here is to further illustrate the great importance electrolytes play to proper physiological functioning, and to show that replacing electrolytes is a crucial element of any endurance athlete’s nutrition routine.
Disclaimer: Contact your physician before starting any exercise program or if you are taking any medication. Individuals with high blood pressure should also consult their physician prior to taking an electrolyte supplement. Overdose of electrolytes is possible, with symptoms such as vomiting and feeling ill, and care should be taken not to overdose on any electrolyte supplement.